NOVA
23 Mar 2016
Jon Palfreman
In 2004, the British chemist Chris Dobson speculated that there might be a universal elixir out there that could combat not just alpha-synuclein for Parkinson’s but the amyloids caused by many protein-misfolding diseases at once. Remarkably, in that same year an Israeli scientist named Beka Solomon discovered an unlikely candidate for this elixir, a naturally occurring microorganism called a phage.
Solomon, a professor at Tel Aviv University, made a serendipitous discovery one day when she was testing a new class of agents against Alzheimer’s disease. If it pans out, it might mark the beginning of the end of Alzheimer’s, Parkinson’s, and many other neurodegenerative diseases. It’s a remarkable story, and the main character isn’t Solomon or any other scientist but a humble virus that scientists refer to as M13.

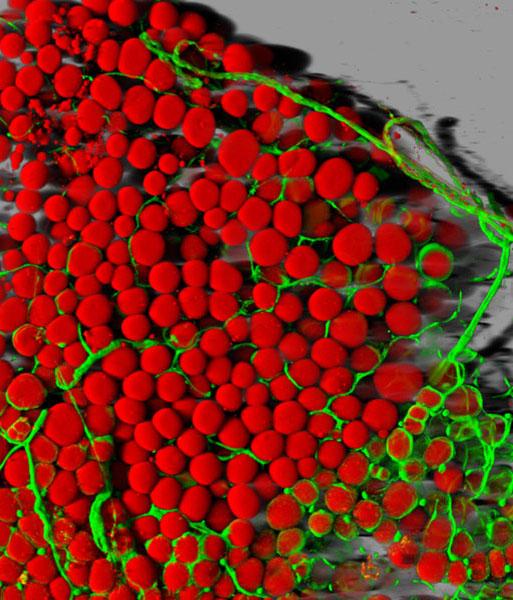
Alzheimer’s disease can cause brain tissues to atrophy, seen here in blue. No image credit.
Among the many varieties of viruses, there is a kind that only infects bacteria. Known as bacteriophages, or just phages, these microbes are ancient (over three billion years old) and ubiquitous: they’re found everywhere from the ocean floor to human stomachs. The phage M13’s goal is to infect just one type of bacteria, Escherichia coli, or E. coli, which can be found in copious amounts in the intestines of mammals. Like other microorganisms, phages such as M13 have only one purpose: to pass on their genes. In order to do this, they have developed weapons to enable them to invade, take over, and even kill their bacterial hosts. Before the advent of antibiotics, in fact, doctors occasionally used phages to fight otherwise incurable bacterial infections.
To understand Solomon’s interest in M13 requires a little background about her research. Solomon is a leading Alzheimer’s researcher, renowned for pioneering so-called immunotherapy treatments for the disease. Immunotherapy employs specially made antibodies, rather than small molecule drugs, to target the disease’s plaques and tangles. As high school students learn in biology class, antibodies are Y-shaped proteins that are part of the body’s natural defense against infection. These proteins are designed to latch onto invaders and hold them so that they can be destroyed by the immune system. But since the 1970s, molecular biologists have been able to genetically engineer human-made antibodies, fashioned to attack undesirable interlopers like cancer cells. In the 1990s, Solomon set out to prove that such engineered antibodies could be effective in attacking amyloid-beta plaques in Alzheimer’s as well.
In 2004, she was running an experiment on a group of mice that had been genetically engineered to develop Alzheimer’s disease plaques in their brains. She wanted to see if human-made antibodies delivered through the animals’ nasal passages would penetrate the blood-brain barrier and dissolve the amyloid-beta plaques in their brains. Seeking a way to get more antibodies into the brain, she decided to attach them to M13 phages in the hope that the two acting in concert would better penetrate the blood-brain barrier, dissolve more of the plaques, and improve the symptoms in the mice—as measured by their ability to run mazes and perform similar tasks.
Solomon divided the rodents into three groups. She gave the antibody to one group. The second group got the phage-antibody combination, which she hoped would have an enhanced effect in dissolving the plaques. And as a scientific control, the third group received the plain phage M13.
Because M13 cannot infect any organism except E. coli, she expected that the control group of mice would get absolutely no benefit from the phage. But, surprisingly, the phage by itself proved highly effective at dissolving amyloid-beta plaques and in laboratory tests improved the cognition and sense of smell of the mice. She repeated the experiment again and again, and the same thing happened. “The mice showed very nice recovery of their cognitive function,” Solomon says. And when Solomon and her team examined the brains of the mice, the plaques had been largely dissolved. She ran the experiment for a year and found that the phage-treated mice had 80% fewer plaques than untreated ones. Solomon had no clear idea how a simple phage could dissolve Alzheimer’s plaques, but given even a remote chance that she had stumbled across something important, she decided to patent M13’s therapeutic properties for the University of Tel Aviv. According to her son Jonathan, she even “joked about launching a new company around the phage called NeuroPhage. But she wasn’t really serious about it.”
The following year, Jonathan Solomon—who’d just completed more than a decade in Israel’s special forces, during which time he got a BS in physics and an MS in electrical engineering—traveled to Boston to enroll at the Harvard Business School. While he studied for his MBA, Jonathan kept thinking about the phage his mother had investigated and its potential to treat terrible diseases like Alzheimer’s. At Harvard, he met many brilliant would-be entrepreneurs, including the Swiss-educated Hampus Hillerstrom, who, after studying at the University of St. Gallen near Zurich, had worked for a European biotech venture capital firm called HealthCap.
Following the first year of business school, both students won summer internships: Solomon at the medical device manufacturer Medtronic and Hillerstrom at the pharmaceutical giant AstraZeneca. But as Hillerstrom recalls, they returned to Harvard wanting more: “We had both spent…I would call them ‘weird summers’ in large companies, and we said to each other, ‘Well, we have to do something more dynamic and more interesting.’ ”
In their second year of the MBA, Solomon and Hillerstrom took a class together in which students were tasked with creating a new company on paper. The class, Solomon says, “was called a field study, and the idea was you explore a technology or a new business idea by yourself while being mentored by a Harvard Business School professor. So, I raised the idea with Hampus of starting a new company around the M13 phage as a class project. At the end of that semester, we developed a mini business plan. And we got on so well that we decided that it was worth a shot to do this for real.”
In 2007, with $150,000 in seed money contributed by family members, a new venture, NeuroPhage Pharmaceuticals, was born. After negotiating a license with the University of Tel Aviv to explore M13’s therapeutic properties, Solomon and Hillerstrom reached out to investors willing to bet on M13’s potential therapeutic powers. By January 2008, they had raised over $7 million and started hiring staff.
Their first employee—NeuroPhage’s chief scientific officer—was Richard Fisher, a veteran of five biotech start-ups. Fisher recalls feeling unconvinced when he first heard about the miraculous phage. “But the way it’s been in my life is that it’s really all about the people, and so first I met Jonathan and Hampus and I really liked them. And I thought that within a year or so we could probably figure out if it was an artifact or whether there was something really to it, but I was extremely skeptical.”
Fisher set out to repeat Beka Solomon’s mouse experiments and found that with some difficulty he was able to show the M13 phage dissolved amyloid-beta plaques when the phage was delivered through the rodents’ nasal passages. Over the next two years, Fisher and his colleagues then discovered something totally unexpected: that the humble M13 virus could also dissolve other amyloid aggregates—the tau tangles found in Alzheimer’s and also the amyloid plaques associated with other diseases, including alpha-synuclein (Parkinson’s), huntingtin (Huntington’s disease), and superoxide dismutase (amyotrophic lateral sclerosis). The phage even worked against the amyloids in prion diseases (a class that includes Creutzfeldt-Jakob disease). Fisher and his colleagues demonstrated this first in test tubes and then in a series of animal experiments. Astonishingly, the simple M13 virus appeared in principle to possess the properties of a “pan therapy,” a universal elixir of the kind the chemist Chris Dobson had imagined.
This phage’s unique capacity to attack multiple targets attracted new investors in a second round of financing in 2010. Solomon recalls feeling a mix of exuberance and doubt: “We had something interesting that attacks multiple targets, and that was exciting. On the other hand, we had no idea how the phage worked.”
The Key
That wasn’t their only problem. Their therapeutic product, a live virus, it turned out, was very difficult to manufacture. It was also not clear how sufficient quantities of viral particles could be delivered to human beings. The methods used in animal experiments—inhaled through the nose or injected directly into the brain—were unacceptable, so the best option available appeared to be a so-called intrathecal injection into the spinal canal. As Hillerstrom says, “It was similar to an epidural; this was the route we had decided to deliver our virus with.”
While Solomon and Hillerstrom worried about finding an acceptable route of administration, Fisher spent long hours trying to figure out the phage’s underlying mechanism of action. “Why would a phage do this to amyloid fibers? And we really didn’t have a very good idea, except that under an electron microscope the phage looked a lot like an amyloid fiber; it had the same dimensions.”
Boston is a town with enormous scientific resources. Less than a mile away from NeuroPhage’s offices was MIT, a world center of science and technology. In 2010, Fisher recruited Rajaraman Krishnan—an Indian postdoctoral student working in an MIT laboratory devoted to protein misfolding—to investigate the M13 puzzle. Krishnan says he was immediately intrigued. The young scientist set about developing some new biochemical tools to investigate how the virus worked and also devoured the scientific literature about phages. It turned out that scientists knew quite a lot about the lowly M13 phage. Virologists had even created libraries of mutant forms of M13. By running a series of experiments to test which mutants bound to the amyloid and which ones didn’t, Krishnan was able to figure out that the phage’s special abilities involved a set of proteins displayed on the tip of the virus, called GP3. “We tested the different variants for examples of phages with or without tip proteins, and we found that every time we messed around with the tip proteins, it lowered the phage’s ability to attach to amyloids,” Krishnan says.
Virologists, it turned out, had also visualized the phage’s structure using X-ray crystallography and nuclear magnetic resonance imaging. Based on this analysis, those microbiologists had predicted that the phage’s normal mode of operation in nature was to deploy the tip proteins as molecular keys; the keys in effect enabled the parasite to “unlock” E. coli bacteria and inject its DNA. Sometime in 2011, Krishnan became convinced that the phage was doing something similar when it bound to toxic amyloid aggregates. The secret of the phage’s extraordinary powers, he surmised, lay entirely in the GP3 protein.
As Fisher notes, this is serendipitous. Just by “sheer luck, M13’s keys not only unlock E. coli; they also work on clumps of misfolded proteins.” The odds of this happening by chance, Fisher says, are very small. “Viruses have exquisite specificity in their molecular mechanisms, because they’re competing with each other…and you need to have everything right, and the two locks need to work exactly the way they are designed. And this one way of getting into bacteria also works for binding to the amyloid plaques that cause many chronic diseases of our day.”
Having proved the virus’s secret lay in a few proteins at the tip, Fisher, Krishnan, and their colleagues wondered if they could capture the phage’s amyloid-busting power in a more patient friendly medicine that did not have to be delivered by epidural. So over the next two years, NeuroPhage’s scientists engineered a new antibody (a so-called fusion protein because it is made up of genetic material from different sources) that displayed the critical GP3 protein on its surface so that, like the phage, it could dissolve amyloid plaques. Fisher hoped this novel manufactured product would stick to toxic aggregates just like the phage.
By 2013, NeuroPhage’s researchers had tested the new compound, which they called NPT088, in test tubes and in animals, including nonhuman primates. It performed spectacularly, simultaneously targeting multiple misfolded proteins such as amyloid beta, tau, and alpha-synuclein at various stages of amyloid assembly. According to Fisher, NPT088 didn’t stick to normally folded individual proteins; it left normal alpha-synuclein alone. It stuck only to misfolded proteins, not just dissolving them directly, but also blocking their prion-like transmission from cell to cell: “It targets small aggregates, those oligomers, which some scientists consider to be toxic. And it targets amyloid fibers that form aggregates. But it doesn’t stick to normally folded individual proteins.” And as a bonus, it could be delivered by intravenous infusion.
The Trials
There was a buzz of excitement in the air when I visited NeuroPhage’s offices in Cambridge, Massachusetts, in the summer of 2014. The 18 staff, including Solomon, Hillerstrom, Fisher, and Krishnan, were hopeful that their new discovery, which they called the general amyloid interaction motif, or GAIM, platform, might change history. A decade after his mother had made her serendipitous discovery, Jonathan Solomon was finalizing a plan to get the product into the clinic. As Solomon says, “We now potentially have a drug that does everything that the phage could do, which can be delivered systemically and is easy to manufacture.”
Will it work in humans? While NPT088, being made up of large molecules, is relatively poor at penetrating the blood-brain barrier, the medicine persists in the body for several weeks, and so Fisher estimates that over time enough gets into the brain to effectively take out plaques. The concept is that this antibody could be administered to patients once or twice a month by intravenous infusion for as long as necessary.
NeuroPhage must now navigate the FDA’s regulatory system and demonstrate that its product is safe and effective. So far, NPT088 has proved safe in nonhuman primates. But the big test will be the phase 1A trial expected to be under way this year. This first human study proposed is a single-dose trial to look for any adverse effects in healthy volunteers. If all goes well, NeuroPhage will launch a phase 1B study involving some 50 patients with Alzheimer’s to demonstrate proof of the drug’s activity. Patients will have their brains imaged at the start to determine the amount of amyloid-beta and tau. Then, after taking the drug for six months, they will be reimaged to see if the drug has reduced the aggregates below the baseline.
“If our drug works, we will see it working in this trial,” Hillerstrom says. “And then we may be able to go straight to phase 2 trials for both Alzheimer’s and Parkinson’s.” There is as yet no imaging test for alpha-synuclein, but because their drug simultaneously lowers amyloid-beta, tau, and alpha-synuclein levels in animals, a successful phase 1B test in Alzheimer’s may be acceptable to the FDA. “In mice, the same drug lowers amyloid beta, tau, and alpha-synuclein,” Hillerstrom says. “Therefore, we can say if we can reduce in humans the tau and amyloid-beta, then based on the animal data, we can expect to see a reduction in humans in alpha-synuclein as well.”
Along the way, the company will have to prove its GAIM system is superior to the competition. Currently, there are several drug and biotech companies testing products in clinical trials for Alzheimer’s disease, against both amyloid-beta (Lilly, Pfizer, Novartis, and Genentech) and tau (TauRx) and also corporations with products against alpha-synuclein for Parkinson’s disease (AFFiRiS and Prothena/Roche). But Solomon and Hillerstrom think they have two advantages: multi-target flexibility (their product is the only one that can target multiple amyloids at once) and potency (they believe that NPT088 eliminates more toxic aggregates than their competitors’ products). Potency is a big issue. PET imaging has shown that existing Alzheimer’s drugs like crenezumab reduce amyloid loads only modestly, by around 10%. “One weakness of existing products,” Solomon says, “is that they tend to only prevent new aggregates. You need a product potent enough to dissolve existing aggregates as well. You need a potent product because there’s a lot of pathology in the brain and a relatively short space of time in which to treat it.”
Future Targets
NeuroPhage’s rise is an extraordinary example of scientific entrepreneurship. While I am rooting for Solomon, Hillerstrom, and their colleagues, and would be happy to volunteer for one of their trials (I was diagnosed with Parkinson’s in 2011), there are still many reasons why NeuroPhage has a challenging road ahead. Biotech is a brutally risky business. At the end of the day, NPT088 may prove unsafe. And it may still not be potent enough. Even if NPT088 significantly reduces amyloid beta, tau, and alpha-synuclein, it’s possible that this may not lead to measurable clinical benefits in human patients, as it has done in animal models.
But if it works, then, according to Solomon, this medicine will indeed change the world: “A single compound that effectively treats Alzheimer’s and Parkinson’s could be a twenty billion-dollar-a-year blockbuster drug.” And in the future, a modified version might also work for Huntington’s, ALS, prion diseases like Creutzfeldt-Jakob disease, and more.
I asked Jonathan about his mother, who launched this remarkable story in 2004. According to him, she has gone on to other things. “My mother, Beka Solomon, remains a true scientist. Having made the exciting scientific discovery, she was happy to leave the less interesting stuff—the engineering and marketing things for bringing it to the clinic—to us. She is off looking for the next big discovery.”
See the full article here .
Please help promote STEM in your local schools.

Stem Education Coalition
NOVA is the highest rated science series on television and the most watched documentary series on public television. It is also one of television’s most acclaimed series, having won every major television award, most of them many times over.

![]()